Ticks are found throughout the United States and can carry many different diseases. Some of the illnesses carried by ticks are easily treated, and some can cause life-long impacts. Unfortunately love for the outdoors puts cavers at extremely high risk for these diseases. Most who cave in tick-heavy areas, such as Southeast Expedition Medical's home region of TAG (Tennessee, Alabama, Georgia), know several people with Lyme disease or Alpha Gal.
Prevention
Perform tick checks several times daily when outdoors.
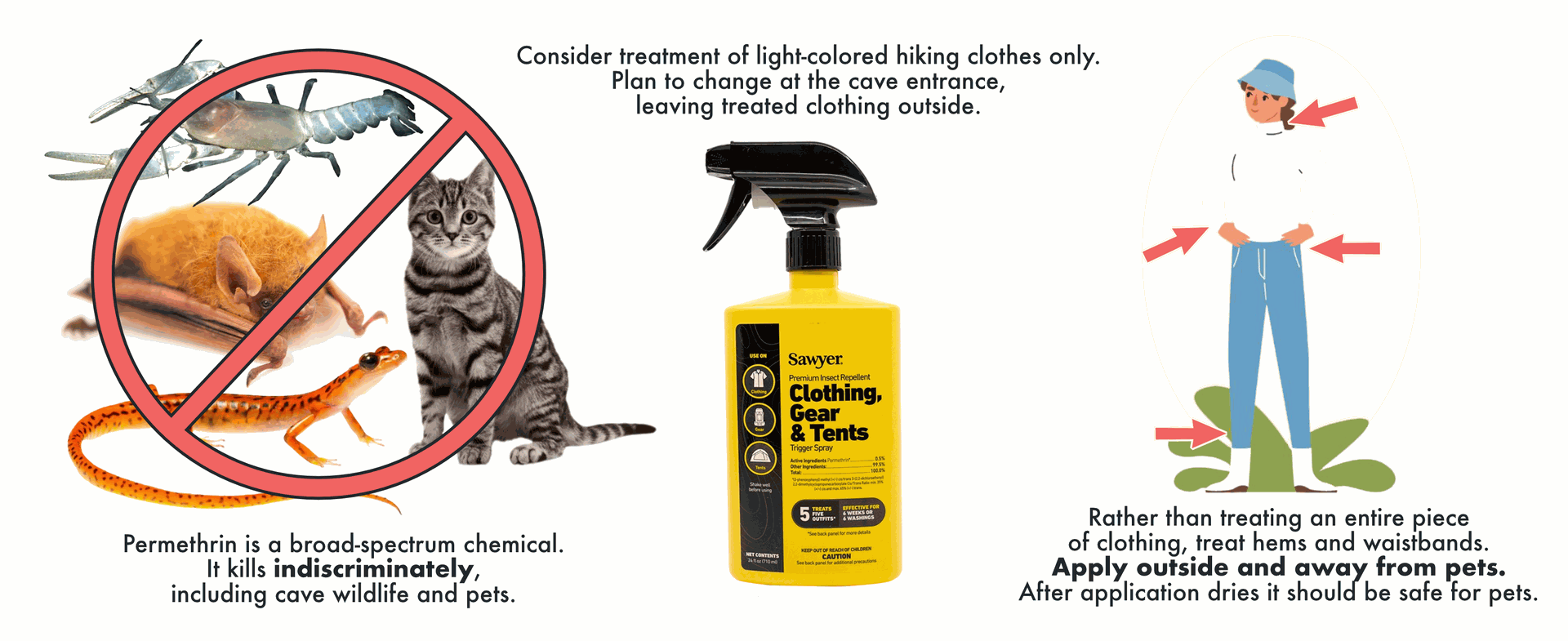
Light-colored shirts and pants help with seeing ticks on clothing.
Use a DEET-based insect repellent.
Treatment of clothing hems with permethrin will kill ticks, and any other wildlife with which it comes into contact. If treating clothing, consider treating hiking clothes and bringing a separate set of clothing for caving. Permethrin-treated clothes will kill cave fauna, such as salamanders, crickets, etc and are a persistent environmental contaminant.
Removal & Initial Treatment
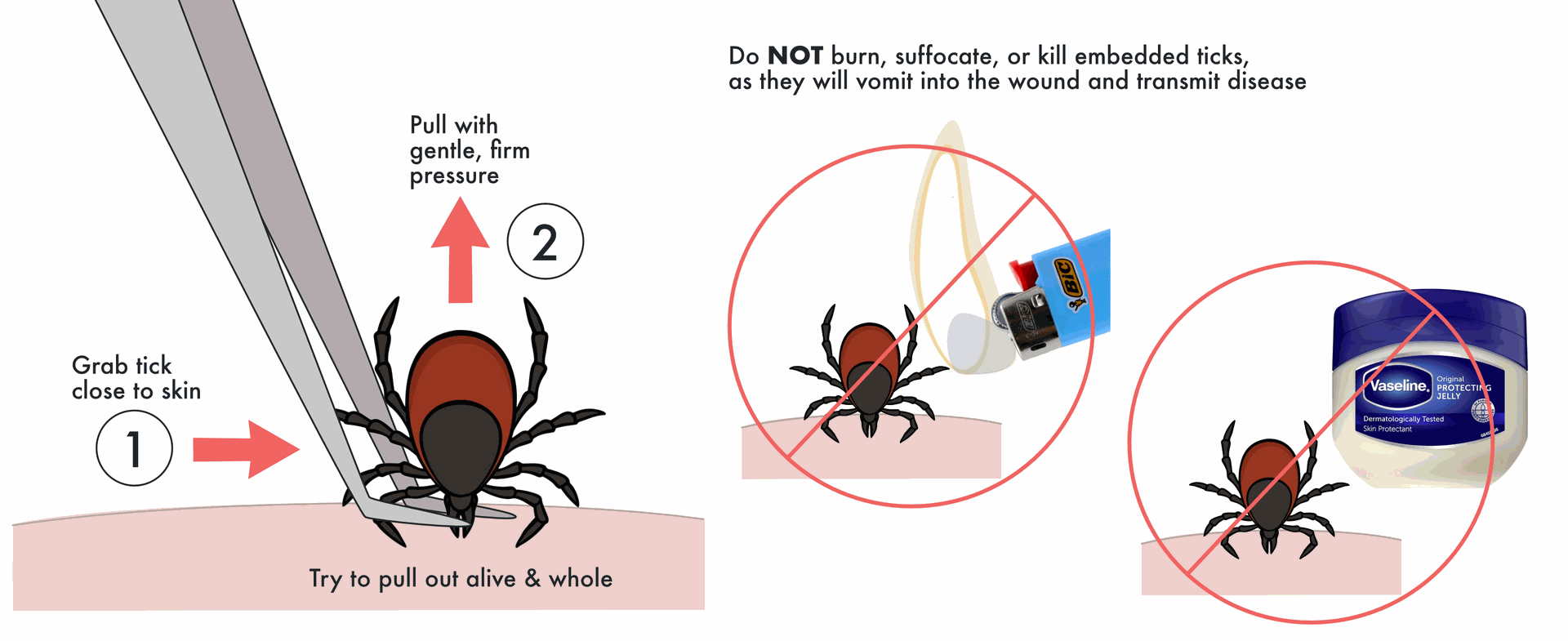
Remove all embedded ticks immediately.
- Grasp as close to the skin as possible and pull with gentle, firm pressure – attempt to pull the whole tick out alive. Use tweezers or a commercial tick removal tool if available.
- Do not burn, suffocate, or kill the tick while embedded – this will cause them to vomit, which could cause disease or infection.
- Place the tick in a sealed container and transport to a fridge or freezer to keep for a few months. At onset of signs & symptoms, the tick can be shipped to a lab for testing.
- Do not crush the tick with your bare finger. This can expose you to blood-borne pathogens. If tick is not retained for testing, drown the tick in alcohol or seal in to a plastic bag & dispose of in municipal waste.
Wash the bite and monitor for signs and symptoms of infection.
Assessment
There are many different types of tick-borne diseases, including:
- Lyme disease
- Rocky Mountain spotted fever (RMSF)
- Alpha-gal syndrome (AGS)
- Anaplasmosis
- Babesiosis
- Bourbon virus
- Colorado tick fever
- Ehrlichiosis
- Hard tick relapsing fever (HTRF)
- Heartland virus
- Powassan virus
- Southern tick-associated rash illness (STARI)
- Spotted fever rickettsioses
- Tularemia
With so many different possible diseases, symptoms can be varied or have odd presentations. However common signs and symptoms to watch for include:
- Fever
- Muscle aches
- Rash
- Fatigue
- Joint pain
Signs and symptoms may appear within a few hours, or they may take weeks or even months to appear. Diagnosis is specialized and can be difficult, so it is strongly recommended to retain the tick for testing.
We understand that the urge to kill embedded ticks is strong, but intact, live ticks are ideal for identification and testing - which can make a significant difference in your outcome if infected.
Testing
Tick testing involves sending a tick to a laboratory to determine if it carries pathogens that can cause diseases like Lyme disease. The test identifies the presence of disease-causing bacteria, protozoa, or viruses in the tick. This information helps assess the risk of infection for a person who has been bitten by the tick. Presence of disease doesn't confirm whether the person has actually been infected, but it does provide a better starting point for medical professionals - speeding up diagnosis and treatment.
How to Store a Tick Prior to Testing
Secure each tick (dead or alive) in a Ziploc bag or other plastic container. Keep the body intact. If the tick is alive then consider double-bagging it for added security and place a slightly damp (1"x 1" small) paper towel in the bag.
- DO NOT
- Wrap the tick in paper or tissue
- Use tape to secure the tick
- Have pooling water or soaking wet paper towel in your specimen bag
- Wrap your tick in a soaking wet paper towel - the contents of your tick will get diluted and lost in the paper towel or pooling water
- DO
- Avoid excess moisture-avoid pooling water or droplets in the bag
- Avoid mold
- Store in the fridge
- Use bubble wrap or other padding for engorged ticks - your mail may go through rollers and large ticks can be crushed
- Double bag or otherwise secure your specimen to avoid escape or damage
When in doubt, sending/storing the tick in a dry bag is preferred.
Common Questions
Should I send my tick via overnight shipping?
The amount of time the tick takes to get to the laboratory will not impact the quality of your test.
After I removed my tick I covered it in alcohol, cooking oil, or another substance. Can it still be tested?
In most cases, yes. PCR tests are robust and will work just fine for most foreign substances. However, bleach, acetone, and other harsh chemicals may limit ability to complete a test. Let the testing service know in a note included with the specimen which chemical(s) were used on the tick so we know the best steps to proceed with the testing.
My tick died after I removed it. Can it still be tested?
PCR testing procedures will work on a tick whether it is alive or not.
My tick broke apart when I removed it. I was only able to save a few pieces. Can it still be tested?
In most cases, yes, they can still test tick parts. However, most disease-causing organisms reside in the salivary glands or gut of the tick. Providing a sample that is only a few legs will probably not give a representative result of what was inside the tick.
How Tick Testing Works
- Tick Submission: You can send the tick to a lab through various channels, like a doctor, a public health department, or a commercial lab.
- Tick Identification: The lab will first identify the tick species under a microscope.
- Pathogen Detection: The lab uses DNA and RNA testing to identify the presence of pathogens.
- Results: The lab sends the results back to the submitter, indicating whether the tick carries any pathogens.
Why Get a Tick Tested?
- Assess Risk:
Tick testing helps determine the risk of infection for a person who has been bitten by the tick. - Inform Treatment:
The results can inform a doctor's decision on whether or not to prescribe preventative antibiotics. - Early Detection:
Testing may allow for early detection of potential infections, potentially leading to quicker and more effective treatment.
Important Considerations
- No Guarantee of Infection:
A positive test result on the tick doesn't guarantee that the person has been infected. - False Positives/Negatives:
There's a chance of false positives or false negatives in testing. - Alternative Testing:
In some cases, your doctor may recommend testing your blood rather than the tick. - Symptoms:
If you develop symptoms after a tick bite, you should consult your doctor, regardless of the tick test results.
Where to Get a Tick Tested
- Commercial Labs: Several labs offer tick testing services, including IGeneX and Ticknology.
- Public Health Departments: Some public health departments offer tick testing services.
- University Labs: University labs, like the University of Maine's Cooperative Extension and the University of Rhode Island also offer tick testing.
What are your best tick tips?
Drop us a comment at info@southeastexpeditionmed.com.
References
- Ticks. CDC. Accessed June 25, 2025. https://www.cdc.gov/ticks/index.html
- Lyme Disease & Tick-Borne Disease Testing. IGeneX. Accessed June 25, 2025. https://igenex.com
- Laboratory Tick Testing. Ticknology. Accessed June 25, 2025. https://www.ticknology.org
- Cooperative Extension: Tick Lab. University of Maine. Accessed June 25, 2025. https://extension.umaine.edu/ticks/submit/
- Tick Encounter. University of Rhode Island. Accessed June 25, 2025. https://web.uri.edu/tickencounter/